
NYT reported on May 3rd that “Mayor Bill de Blasio is championing a plan that would make New York City a pioneer in creating supervised injection sites for illegal drug users, part of a novel but contentious strategy to combat the epidemic of fatal overdoses caused by the use of heroin and other opioids.”
Before going into the merits of such facilities, let’s note that supervised injection facilities are not truly a “novel” strategy. The first facility that had professional staff and allowed injection drug use on site, but wasn’t called a supervised injection facility, opened in the 1970s in Rotterdam (Netherlands). In late 1980s, a cafe in Bern (Switzerland) set up for drug users (IDUs) evolved into the first supervised injection facility. Now Europe has supervised injection sites (also called drug consumption rooms in Europe) all over (see map below). Australia opened its first one in Sydney in 2001. North America got its first one in Vancouver in 2003.

The NYT report goes on to describe that this would be a 12-month pilot program of 4 sites and describes how this would work:
At the sites, which would be called Overdose Prevention Centers, trained staff would be available to administer medications, such as naloxone, to counteract drug overdoses. Social workers would also be on hand to possibly counsel drug users in the hope that they could be steered into programs intended to help them with their addiction.
The sites would be financed and run by nonprofit groups authorized by the city, and may be located within social service providers that already operate needle exchange sites.
In a country in its 114th year of an unwinnable drug war, the report still drew responses from people opposed to the idea.
One commenter said, “Can we please stop enabling and make individuals responsible for their actions! These sites will merely provide emergency medical response in the event of an overdose or tainted/pure supply of the opioid. Onsite counselling? — do you believe an addict wants to be told that what they are doing is dangerous? They’d rather find that alley or isolated spot than to listen to your preaching. If they wanted it, they’d be searching for rehab already!”
Another one said, “Enabling addicts to continue ruining themselves and who contribute nothing to the society and taxpayers who are forced to support their addiction does absolutely nothing to solve the problem.
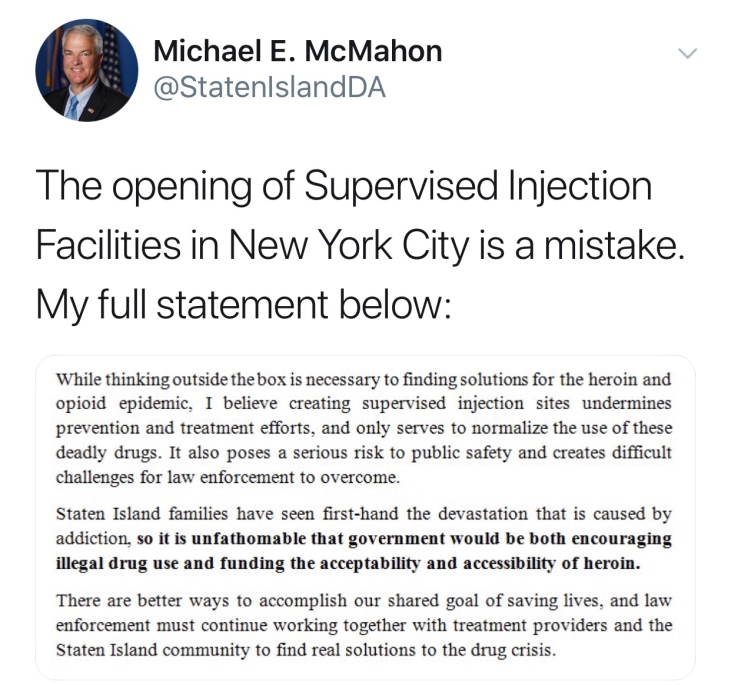
The Staten Island District Attorney responded on Twitter:
Given that supervised injection facilities are not really a new idea, what does research tell us about them? Are the objectors right? Do they (the facilities) normalize the use of deadly drugs? Do they or do they not encourage people with addiction to consider recovery? Are they a drain on the taxpayer?
Regarding the outcomes of Sydney’s Medically Supervised Injection Centre (MSIC), as they are called in Australia, the Australian Alcohol and Drug Foundation reported that by 2015:
- More than 965,000 injections have been supervised
- Management of more than 5,925 overdoses without a single fatality.
- Over 15,300 people have registered to use the centre since opening.
- 70% of the people visiting MSIC had never accessed any local health services prior to visiting the centre.
- More than 12,000 referrals have been made to external health and social welfare services.
- The number of ambulance call outs to Kings Cross has reduced by 80% since MSIC opened.
- There has been no increase in crime in the Kings Cross area.
- The Kings Cross MSIC has been independently evaluated multiple times. All results show the centre is successful and cost effective.
- The number of publicly discarded needles and syringes halved in Kings Cross after the opening of MSIC.
One evaluation of Vancouver’s supervised injection facility after its first 3 years of operation found that:…”the program has been successful in attracting IDUs in the community who have a number of characteristics associated with an increased risk of HIV infection and overdose, as well as IDUs who were more likely to inject drugs in public. In turn, there have been large reductions in public drug use, publicly discarded syringes and syringe sharing after the facility opened. Use of the facility has also been associated with increased uptake of detoxification services; the facility has been a central referral mechanism to a range of other community and medical resources and a key venue for education about safer injecting. Research has indicated that the facility has not resulted in increases in drug dealing in the facility’s vicinity, in drug acquisition crime or in rates of new IDUs or relapse into injection drug use among former IDUs.”
An analysis of the impact of Vancouver’s supervised injection facility on overdose-mortality found that overdoses fell by 35% in a 3 mile radius around the facility, while dropping only about 9% in the rest of city.
Okay, so there are a bunch of positive health outcomes related to supervised injection facilities. What about their cost to the taxpayer. Fortunately, this topic has also been studied. In Vancouver, the supervised injection facility is estimated to have net savings of $18 million over 10 years. A cost-benefit analysis of a potential supervised injection facility in San Francisco found that…”each dollar spent on a SIF would generate US$2.33 in savings, for total annual net savings of US$3.5 million for a single 13-booth SIF.” A similar analysis for a hypothetical supervised injection facility in Baltimore concluded that,…”for an annual cost of $1.8 million, a single SIF would generate $7.8 million in savings, preventing 3.7 HIV infections, 21 Hepatitis C infections, 374 days in the hospital for skin and soft-tissue infection, 5.9 overdose deaths, 108 overdose-related ambulance calls, 78 emergency room visits, and 27 hospitalizations, while bringing 121 additional people into treatment.” The CDC calculates that just preventing one HIV infection saves almost $400,000. Another study estimates that preventing one Hepatitis C infection saves almost $65,000.
In summary, supervised injection facilities:
- Reduce suffering
- Save lives
- Save money
The Staten Island DA is wrong to oppose them and Mayor DeBlasio is right give them a shot (no pun intended).