
Stigma about proven OUD (Opioid Use Disorder) treatments is a significant barrier to getting the opioid crisis under control. Stigma prevents patients from seeking treatment with Suboxone and methadone. And stigma prevents addiction care providers from using Suboxone, methadone, and naloxone.
Stigma in healthcare about medications for OUD is a big part of what keeps the American opioid epidemic going. First, let’s look at the ubiquity and pervasiveness of its effects.
Most Residential Treatment Facilities Do Not Treat OUD with Suboxone
Can you imagine a treatment setting for the most severe cases of any illness caring for patients without using every evidence-based tool available to it?
In 2007 under 20,000 American lives were lost to an opioid. Unfortunately, this number rose to about 45,000 by 2018. They are now at about 67,000. As the crisis deepens, one imagines that medicines proven to treat addiction and save lives would see dramatically increased use, especially in the most intensive treatment settings. Indeed, this study shows that the availability of Suboxone in residential, intensive outpatient, and non-intensive SUD treatment about doubled from 2007 through 2018. 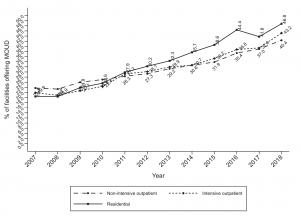
However, the same study shows the use of Suboxone stalled in all settings examined.
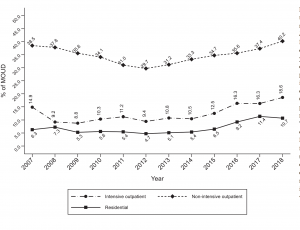
An extensive study of the effectiveness of various treatment pathways for OUD found only Suboxone/methadone treatment reduces overdoses, hospitalizations, and ER visits related to opioid use. However, if you enter residential treatment for OUD, your chances of receiving this proven treatment are only about one in ten.
Furthermore, if you are receiving treatment with Suboxone, most residential programs either will not accept you for treatment. They will instead require stopping the Suboxone before you enter treatment. Salvation Army, which does a lot of good work with individuals with addiction, is now facing a class-action lawsuit because of precisely this ridiculous practice.
All Pharmacies Don’t Carry/Dispense Suboxone
Imagine a diabetes patient in an area with high rates of obesity and type 2 diabetes who goes to a local pharmacy to pick up his insulin. The pharmacy says to him, “Sorry, we don’t carry insulin.” Ever heard of that? Because it doesn’t happen with medications for diabetes, heart failure, high blood pressure, depression, or even pain.
Recently I heard of a group of emergency room physicians saying that they can’t give Suboxone to patients who came in with opioid overdoses. They said it is because their hospital pharmacy does not carry this medicine. I found it hard to believe until I found this study of pharmacies in counties with higher-than-national-average opioid overdose death rates. It shows that only 73% of those pharmacies dispense buprenorphine. Imagine more than 1 in 4 pharmacies refusing to issue insulin or blood pressure medicine. It just doesn’t happen.
Naloxone Dispensing is Less Than 7% of Recommended Levels
Naloxone reverses opioid overdoses and saves lives. The 2016 CDC Guideline for Prescribing Opioids for Chronic Pain recommends prescribing naloxone to individuals at high risk of opioid overdoses. Almost all states have made it possible to get the medication without a prescription. Most insurance companies cover it. By this stage of the opioid epidemic, every at-risk patient should have naloxone handy. Yet, the CDC found that in 2018, the number of doses of naloxone dispensed was 1/16th or about 7% of what it should have been if everyone followed the CDC recommendations about naloxone. Many addiction care providers believe that giving naloxone to opioid-addicted patients enables their addiction. They don’t care that it will let them survive overdoses.
Most Suboxone Waivers are Way Underused
The law requires physicians and others who prescribe Suboxone to get special training, and following that, they have to obtain a special waiver from the DEA (Drug Enforcement Agency) to prescribe it. The DEA then limits their Suboxone caseloads to 30, 100, or 275 patients a month. The actual number depends on prescriber qualifications, setting, and duration for which they have had the waiver.
A 2010 survey of physicians with the waivers found that their average caseload of Suboxone patients was only 26. In addition, a quarter of waivered doctors had not written a single prescription for Suboxone. In a world without stigma, the continuing opioid crisis would lead more healthcare providers to use this lifesaving medication.
Yet, a study published this month that tracked prescribing patterns over six years finds that almost 84% of waivered prescribers (including all disciplines) treat no more than 1-2 patients with Suboxone for several months before stopping altogether.
Let’s Add It All Up
Extraordinary evidence and expert consensus support the use of Suboxone and naloxone in OUD. Yet, patients with OUD can’t find doctors or residential treatment centers willing to treat them with Suboxone. Sometimes, they manage to find doctors who prescribe the medicine. Then they may run into pharmacies that don’t stock or dispense the drug. Let’s say they succeed in getting the medication. But then, if they need residential treatment, they have to stop it again. Once again, they are at high risk of an overdose. But almost nobody thinks to recommend that they keep naloxone handy.
Multiple opportunities to save lives are lost because healthcare professionals can’t overcome the stigma in their hearts and minds. And the opioid epidemic continues to kill.
[Featured image by Kleiton Santos from Pixabay]
[Suboxone is a registered trademark of Indivior]

1 thought on “The Hidden Stigma That Kills People With Opioid Addiction”